Return to Cryoglobulinemia Home Page | Comments on this Web page?
Measuring the Cryocrit in Cryoglobulinemia
Comments by Lee Altenberg. Revised August 8, 2014 .
Because cryoglobulins are thermally unstable, any test that measures the quantity of cryoglobulins in the blood must be performed immediately at the place where the blood is sampled. Tests to measure cryoglobulins can only be sent out to another lab if the lab that drew the blood from the patient immediately separated the serum from the blood cells before sending it out. Otherwise, even if an outside laboratory claims to measure cryoglobulins, any samples sent to it will be invalid because they cannot be processed according to the necessary steps (below). In that case, not only will the quantities of cryoglobulins measured be incorrect, but the test may completely fail to even detect cryoglobulins. Without accurate measurement of cryoglobulin levels, no correct assessment can be made of a patient's treatments.
Therefore, cryoglobulinemia patients must be sure that the lab where their blood is drawn can itself separate the blood cells from the serum at 37°C. Unfortunately, because of the rarity of cryoglobulinemia, most physicians are unaware of the requirements for valid cryoglobulin tests. Fortunately, the Cryocrit test can be performed with the equipment that most any medical testing laboratory has, and should cost only about $20 per test. The only item that may not be immediately available is a 37°C incubator to put the centrifuge inside of. Instead, the centrifuge can be placed in a 37°C walk-in room.
Below are the instructions used by
a hospital that treats many cryoglobulinemia patients (the supervisor of the laboratory requested that the identity of the hospital not be divulged, as the questions they have received regarding cryocrit measurements have been burdensome).
Disclaimer: Anyone wishing to authorize the use of the protocol below with human subjects should
ask their physician to contact me, and I can direct the physician to the laboratory that uses this protocol, and the physician can initiate any necessary exchange of information. This Web page is not an official publication and is for information purposes only.
[Transcribed by Lee Altenberg from the hard copy]
Cryoglobulin Assay
Revised 3/24/97
INTRODUCTION
Cryoglobulins are predominantly immunoglobulin complexes that precipitate out at reduced temperatures and redissolve at some point as the temperature is raised. They are classically said to precipitate at 4°C and redissolve at 37°C. However, these two temperatures are generalizations and varying temperatures are actually observed. The name cryoglobulin is descriptive, since they are observed at cold (cryo) temperatures and involve immunoglobulins as the sole or one of the major components. Other proteins may be involved such as hepatitis B antigen, hepatitis C, fibrinogen, DNA, bovine serum albumen, and complement components (Freedman, 1971, p. 619).
Characteristics of Cryoglobulin
The following is primarily a list of physiochemical and immunochemical characteristics given by McIntosh and Grey (Miescher and Muller-Eberhard, 1976, pp. 619-622).
The conditions under which cryoprecipitation occurs vary from one protein to the next. ``The most important variables appear to be temperature, protein concentration, pH and ionic strength. Under physiologic conditions of pH and ionic strength, protein concentration is the most important factor in determining the temperature at which a particular cryoglobulin will precipitate. In general, the higher the protein concentration, the higher the temperature at which precipitation occurs. The critical temperature for cryoprecipitation varies widely. Cryoprecipitation may occur close to body temperature, whereas in other cases cryoprecipitation does not occur above 5°C.'' (Immunopathology has observed one cryoglobulin that precipitated slightly at 37°C and produced a considerable precipitate at 35.5°C.)
``The physical characteristics of the cryoprecipitate also differs from one protein to the next; in some cases a gelatinous precipitate is formed, whereas in others it is flocculent and in some cases crystalline. Also, the form of the precipitate may vary within a given cryoglobulin depending upon the pH and ionic strength conditions used during the cyroprecipitation.''
Types of Cryoglobulin
Cryoglobulin can be placed into three general types based on immunoglobulin compositions.
- MONOCLONAL (pure) = one homogeneous immunoglobulin present in the cryoprecipitate. (e.g., only monoclonal IgM Kappa present). Usually found in multiple myeloma, Waldenstrom's macroglobulinemia and lymphoma.
- MIXED WITH ONE MONOCLONAL = has two or more immunoglobulins present, and one of them is monoclonal with Rheumatoid Factor activity. About half of the patients have underlying lymphoid neoplasms. Common in hepatitis C and Sjogren's syndrome.
- MIXED - POLYCLONAL = More than one immunoglobulin present with no monoclonality. Usually seen in the connective tissue diseases or chronic infections.
``Any of the major immunoglobulin classes may be found in each of these three types, and Bence-Jones proteins have also been observed in the monoclonal type. In some cases it may be difficult to distinguish between the first two types of cryoglobulinemia, since in many instances a monoclonal protein is the major component present in the mixed type and the polyclonal component may be missed if very careful antigenic analysis is not carried out.'' (Freedman, 1971, p. 619).
Disease States
Cryoglobulins are described in many clinical conditions such as lymphoproliferative disorders, viral infections, and connective tissue diseases. Physical findings on patients with cryoglobulinemia may include purpura, vasculitis with multisystem involvement, glomerulonephritis, synovitis with joint swelling and pain and serositis-pleural effusion and pain (Nakamura, 1974, p. 168).
Supplies
- Centrifuge at 37°C.
A small table top centrifuge in a large 37° incubator will work.
- Centrifuge, 4°C.
- Tubes for cryocrits – Disposable Hematocrit tubes, with calibrations from 1 to 100.
- Tubes, 15 ml centrifuge
- Water bath, 37°C.
- FTA Hemagglutination Buffer, BBL/BD #11248, Fisher Scientific
Solutions
FTA Hemagglutination buffer
- Reconstitute by directions on container (the amounts vary slightly from one batch to another).
0.05 M Phosphate buffer, pH 7.0 – Wash Buffer
- 160 ml FTA Hemagglutination Buffer.
- 288 ml deionized water
- Store at 4°C
- (Note: Higher salt contents will tend to dissolve the precipitate).
Specimen Collection and Handling
Cryoglobulins come out of solution below body temperature.
Serum must be obtained from clotted blood maintained at body temperature, from time of withdrawal.
If blood is kept at lower temperatures, the cryoprecipitate may centrifuge out with the blood clot.
The following procedure must be followed or the specimen is NOT acceptable.
- CAUTION: Specimen is not acceptable when drawn on a patient receiving heparin or any other anti-coagulant.
When a Dialysis/Apheresis patient has a catheter with heparin, 10 ml or more must be wasted (discarded) before specimen for Cryoglobulin is drawn.
Peripheral stick is preferred.
(Heparin is anti-Complementary and will therefore breakdown the Cryo immune complexes which contain complement producing a false negative or reduced Cryocrit.)
Other anti-coagulants chelate Ca and deplete complement
- Prepare transporting chamber:
- Select a receptacle that will maintain a fairly constant temperature.
(Patient's styrofoam pitchers with lids work very well)
- Insert a thermometer, QC'd at 37°C, through the lid.
- Add body temperature water to the receptacle.
Start with water at 39°-41°C, so the temperature will not be below 37°C when received in the lab.
- Use vacutainers, not glass syringes, to draw the blood.
- Collect 20ml in red tops and place immediately into transporting chamber. If other tests are to be run in Immunopath, place all of the blood into the 37°C chamber.
- Deliver to lab immediately.
- Reject any specimen which does not comply with all of the criteria listed above. The specimen must be redrawn and must comply with all requirements.
Specimen Processing
- Blood received in the lab must be at 37° to 41°C.
If it is at any other temperature:
Reject the specimen. It must be redrawn (see specimen collection section).
- Place immediately into 37°C water bath
Let set for 30 minutes or until clotted.
- Spin in 37°C centrifuge/2000 rpm/5 min.
- Immediately withdraw all serum and place into centrifuge tubes.
- Spin again in 37°C centrifuge/2000 rpm/5 min. (to make sure all RBC's and fibrin are spun out).
If question possible RBC's after 2nd spin – spin a third time.
(Careful not to over heat specimen)
- If a clot forms in the serum (during the second spin), there is anticoagulant in the specimen. See specimen collection section, steps 5 and 6.
The specimen must be rejected.
- Label tubes:
- Two 15 ml graduated centrifuge tubes.
- One cryocrit tube.
- If other tests were ordered label these and 2 stocks tubes.
- If no other tests ordered, label 4 tubes to be placed in specimen stock rack.
- Immediately, after the last spin, transfer the serum to the labeled centrifuge tubes.
- There should be 4ml or more of serum in each tube.
Less can be accepted but, if there is any question on the results, a larger specimen may be required.
- Toss precipitate
- Promptly, fill the cryocrit tube to the 100 mark with serum from a centrifuge tube..
- Place at least 100 micro L into each of the 4 stock tubes and/or the tubes for other tests.
- Place the 3 cryo tubes at 4°C.
Place other tubes in their appropriate rack for test ordered and/or in stock freezer.
NOTE: When cryoglobulin is positive and other Immunopath tests ordered:
Run all other tests on the properly collected and handled at 37°C specimen. (Antibody activity could be tied up in the cryoprecipitate)
EXCEPT – do NOT run a specimen with cryoglobulin in the ARRAY. For the Array – use supernatant off of the cryo, or serum from a routine collection and spin the serum again just before placing on the Array.
Procedure
- Cryoprecipitation can start within an hour or take several days.
Observe the specimen daily for up to 5 days.
If there is a question at any step, consult supervisor.
- If the serum remains COMPLETELY CLEAR for 5 days, report Negative.
- If the serum becomes SLIGHTLY CLOUDY after 2-5 days:
- Centrifuge the control tube at 4°C/2000 rpm/10 min.
If a precipitate does not form, report as Negative at 5 days.
- If a precipitate does form, ring the tube at the top of the precipitate with a marker and place tube in 37°C waterbath.
Let set for 1-18 hours.
If a precipitate does not dissolve, report as Negative at 5 days.
- If a precipitate does dissolve, label tube ``4°C to 37°C'' and place back at 4°C.
If precipitate reforms, report as Positive.
- If a specimen becomes DEFINITELY CLOUDY (with visible precipitate):
- Place Control tube in 37° waterbath.
Check at about 1-4 hours.*
If it clears – place tube back at 4°C.
If precipitate reforms, report as Positive.
- *If, after the 1-4 hours, it does not clear, leave for overnight.
Compare the control with the 4°C ``test'' tube to decide if partial clearing occurred.
If no clearing occurred, place control back at 4°C. (See Note #1)
At 5 days, spin ``test'' at 4°C.
If no precipitate forms, report as Negative.
- If a precipitate forms, ring tube at top of precipitate and place into a 37°C waterbath for overnight.
If it does not dissolve, report as Negative, at 5 days.
- If it does dissolve, place back at 4°C.
If precipitate does not re-form, report as Negative.
- If a precipitate does re-form, report as Positive.
See Notes 1, 2, and 3.
- Note #1.
- Some cryoglobulin must be warmed to greater than 37°C to dissolve.
If a definite flocculent cloudiness is seen which does not redissolve when placed at 37°C for overnight, perform the following:
- Set up a pan of water on hot plate.
Start with 37°C water.
- Check the temperature with a thermometer.
(Do not let thermometer rest on bottom of pan).
- Hold the control tube in the water and slowly increase the temperature.
(Do not let tube rest on bottom of pan, next to hot plat)
- Record the temperature when the specimen clears.
Usually 40-45°C is sufficient.
Never heat past 63°C for 3 minutes.
- Note #2.
- Rarely a precipitate will appear to partially redissolve when placed at 37°C.
(There could be a small cryoglobulin and a little fibrin)
- Spin control tube which has been at 37°C for overnight, in 37°C centrifuge for 8 minutes.
- Carefully, withdraw the supernatant and place it into a separate tube labeled ``37° super''.
(If a cryo is actually present it should be dissolved in this supernatant and the other non-cryo precipitate should be left as sediment – label as ``sediment after 37° spin'').
- Place the `37° super'' at 4°C for 24-48 hours.
- Spin at 2000 rpm/4°C/8 minutes.
- If there is a precipitate, report as Positive.
Cryocrit will have to be estimated from this tube.
- Note #3.
- If, for some reason there is still a questionable cryoglobulin, set up the Immunofixation (see Characterization – Immunofixation).
If immunoglobulins are present and albumin absent in the precipitate the cryoglobulin is Positive.
If no immunoglobulins are present, the cryoglobulin is Negative.
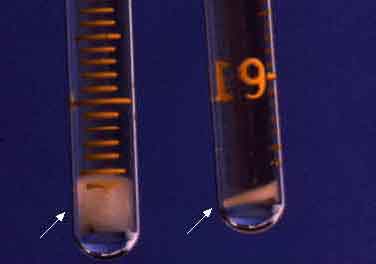
Determine Cryocrit Percent
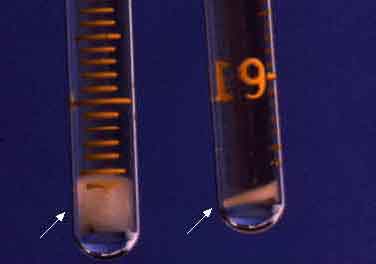
- Determine percent CRYOCRIT on all positive cryoglobulins.
- Spin cryocrit tube at 2000 rpm/4°C/10 min.
- Determine percent by reading calibrations from 1 to 100.
- If crit is <= 2%, report.
- If crit is greater than 2%, centrifuge for another 20 minutes.
(Large cryocrits need 30 minutes to sufficiently pack)
Rare Atypical Cryocrit
We have seen a rare atypical Cryocrit which will not spin down after 30 min/2000 rpm. This is apparent because there will be an obviously false high Crit (e.g.: 50%) after the 30 min. spin.
When this is seen, take the following steps:
Characterization – Immunofixation
Characterize all Positive cryoglobulins.
Run Immunofixation to determine immunoglobulins present and possible presence of monoclonality.
Run RF to see if the cryoprecipitate contains Rheumatoid factor (anti-immunoglobulins) activity.
- Specimen preparation for IFX and RF:
- Centrifuge the 4°C ``test'' tube at 2000 rpm/4°C/8 minutes.
Draw off supernatant serum and place into another tube and label as ``Super''.
Label the tube with the centrifuged precipitate as ``Precip''.
- RF:
Place an aliquot of the super into a small specimen tube for RF and label well.
Obtain a frozen aliquot of whole 37°C collected serum.
Place both the ``Super'' aliquot and the frozen aliquot into the rack for RF.
Place the rest of the ``Super'' back into the cryo cup at 4°C.
- Wash the precipitate to prepare for Immunofix:
Wash the precipitate with 0.05 M Phosphate Buffer, 2000 rpm/4°C/10 min.
Wash 5 times.
(If the precipitate is so small that it is easily washed away, wash 4 or 3x.)
Remove last wash supernatant as completely as possible.
- Redissolve cryoprecipitate:
Add 0.85% saline – usually 25 microliters to 500 microliters, depending on the amount.
Careful – Do not add too much saline – start with 25 microliters.
If not ready to set up IFX, set Precip in cryo cup at 4°C.
- SET UP IFX ON ``Precip'' and ``Super''
See HRE/IFE Procedure Manual – ``Immunofixation for Cryoglobulin by Beckman Paragon'' procedure.
Results Reports
NEGATIVE – REPORT
ALL POSITIVE CRYOGLOBULINS:
Consult supervisor or director before putting out final reports.
Write up all results on Cryo Patient sheets.
File the Cryo Patient sheets in the Cryo notebook.
FOLLOW-UP CRYOCRITS
Report repetitive follow-up cryocrits on known positives at 24 hours.
Record results on Cryo Patient sheets.
NOTES
Complement Dependence can be determined.
- Spin an aliquot of the 4°C specimen.
- Ring the meniscus of the precipitate with a marking pen.
- Place at 56°C for 30 minutes.
(To break down complement)
- Place specimen back at 4°C for overnight or whatever time it took the original cryo to precipitate.
- Spin at 2000 rpm/4°C/8 minutes
If precipitate reforms, cryoglobulin is not complement dependent.
If it does no reform, it is complement dependent.
If it partially reforms (precipitate forms, but is below the ring from step b.), then it is partially complement dependent.
REFERENCES
- Bloch, Durt J., ``Cryoglobulinemia and Hepatitis C Virus,'' New England Journal of Medicine, Vol. 327, pp 1521-1522, November 19, 1992.
- Cohen, Alan S. (ed) Laboratory Diagnostic Procedures in the Rheumatic Diseases. Little, Brown and Company, Boston. pp. 123, 1975.
- Freedman, Samuel O.
Clinical Immunology. Harper and Row, New York. pp. 336-337, 1971.
- Miescher, Peter A. and Muller-Eberhard Hans J.
Textbook of Immunopathology. Grune and Stratton, New York. pp. 619-627, 1976.
- Mussett, Lunel F., et al. "High Incidence of Cryoglobulinemia in Chronic Liver Disease, Z" CAP Today, p. 6, December 1194.
- Nakamura, Robert M.
Immunopathology, Clinical Laboraotry Concepts and Methods. Little, Brown and Company, Boston. pp. 168-191, 1974.
- Samter, Max, et al. (ed), Immunological Disease, Little, Brown & Company, Boston, pp 1687-1702, 1988.
- Stites, Daniel, John Stobo, Vivian Wells, Basic and Clinical Immunology, Appleton & Lange, Norwalk, Connecticut, pp. 25-256, 1987.
Return to Cryoglobulinemia Home Page